Dr. Ezekiel Emanuel Offers a Compelling Argument
What will the future of healthcare look like? It’s an issue that public affairs commentators and policymakers across the political spectrum continue to debate.

In 1994, the late Dr. William Kissick, a professor emeritus at Wharton and the University of Pennsylvania Schools of Medicine and Nursing, identified three competing issues that the healthcare industry has struggled to address effectively. These issues – access, quality and cost containment – what Dr. Kissick called the “Iron Triangle of Healthcare,” continue to perplex policymakers and healthcare decision-makers to this day.
Recently one of the nation’s leading healthcare policy experts, Ezekiel J. Emanuel, MD, PhD, Vice Provost for Global Initiatives and Chair of the Department of Medical Ethics and Health Policy at the University of Pennsylvania, offered some important insights into where the national healthcare system is heading, and what it might mean for the Philadelphia region. In part he rejected the conventional notion that it is possible for health care systems to only achieve two of the three parts of the Iron Triangle. He argued all three had to be achieved together. It was all part of a symposium on “Shaping Health Care” sponsored by the Chamber of Commerce for Greater Philadelphia and The Wistar Institute.
Lowering Costs
Finding a way to provide high-value care for all Americans – namely care marked by high quality and low costs with universal coverage – is a goal shared by providers and policymakers alike. According to Dr. Emanuel, “the only way to lower healthcare costs is to change the delivery system to ensure high quality care.”
Traditionally, one of the most significant contributors to the high cost of healthcare has been the combination of providing unnecessary services and inefficiency in how necessary healthcare services are delivered. One example is standardization of practices so everyone – from physician to nurse to medical assistant – handles the same complaint according to agreed-upon guidelines. For instance, physicians in one local oncology practice were treating mouth sores after chemotherapy in different ways. The practice standardized to one optimal practice that everyone followed.
Another common example is the fact that some health care groups allow their physicians to control their schedules, leading to double-booking, limited hours, and an inability to work around no-shows or walk-ins.
Creating Efficiencies
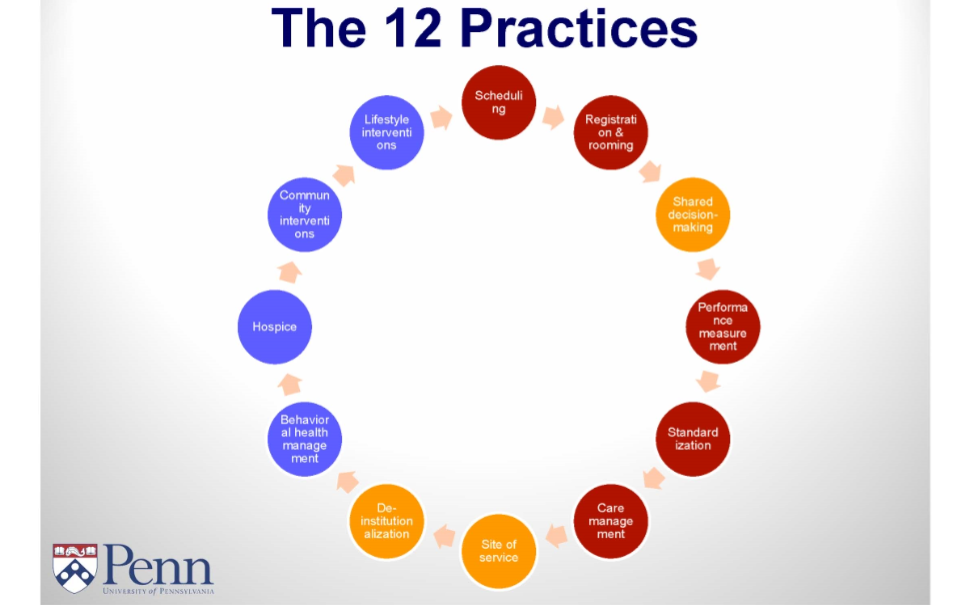
Dr. Emanuel identified 12 transformational practices that he says can help physician practices and healthcare organizations improve the quality and cost of care they provide to their patients:
- Scheduling
- Registration & rooming
- Shared decision-making
- Performance measurement
- Standardization
- Chronic Care management
- Site of service
- De-institutionalization
- Behavioral health management
- Hospice
- Community interventions
- Lifestyle interventions
Many of these practices will improve efficiencies – lowering per unit costs by finding ways to improve a healthcare process or system, or working in collaboration with partners in a way that benefits all involved parties. Others will eliminate unnecessary and undesired services – lowering total costs.
Even seemingly minor changes can show major results. For example, streamlining scheduling practices can offer several benefits: 1) It allows practices to accommodate walk-ins without long wait times instead of sending them to the more expensive emergency room; 2) it increases provider efficiency, as physicians no longer double book or adjust schedules; and 3) it decreases the amount of time wasted due to missed appointments.
Similarly, Dr. Emanuel noted that transformational organizations are providing more services, such as palliative care, in the home. This care is initiated well before a patient becomes terminally ill and is ready for hospice. This approach elicits patients’ preferences for life-sustaining treatments, such as respirators, ICU admission, or dialysis, and tries to keep them at home for the last year of life. It also makes transitioning to hospice in the last weeks of life less abrupt. All these changes lead to care that is both less costly and more in accord with patients’ wishes.
Performance Measures
The pathway for healthcare providers to truly transform also involves the use of real-time performance measures, Dr. Emanuel said. Standardizing clinical practices and treatment procedures based on measurable qualitative data is vital to reducing costs and improving outcomes.
While some physicians may insist that “their” way is the best, organizations need to convince them to adhere to guideline-driven standards. Paradoxically, one effective way to persuade doctors to adapt to standardized measures is to task them with developing the standardized practices and encourage adherence through financial incentives.
At the same time, organizations need to improve their risk adjustment skills in order to continue to improve their healthcare management practices. Risk adjustment is defined as “a statistical process that takes into account the underlying health status and health spending of the enrollees in an insurance plan when looking at their healthcare outcomes or healthcare costs.” This ensures physicians who see sicker patients are not penalized.
The ultimate goal is to transform the U.S. healthcare structure into a truly patient-centered, efficient and cost-effective system. Dr. Emanuel notes that the Philadelphia region is a leading example of how organizations are learning to work together to achieve those goals. He said he is confident that by 2030, the entire world will be looking at the United States to understand how healthcare transformation is accomplished.