All Hands on Deck Against the Opioid Threat
One of the most serious public health issues facing us today is the opioid crisis. As the crisis has continued to grow over the course of the past decade, its impact is far-reaching in terms of financial losses as well as human costs.
As medical professionals and public policy officials strive to find answers to this continually growing problem, it is incumbent on healthcare communicators to be ready to work with their respective partners to develop strategies to reach out and bring together those impacted by this dreadful epidemic – not only abusers, but loved ones, family members, healthcare professionals, community leaders, elected officials and more.
Opioid Crisis by the Numbers
In November, a report from the Council of Economic Advisers estimated that in 2015, the economic cost of the opioid crisis was $504 billion, or 2.8% of the nation’s Gross Domestic Product that year. That number was more than six times larger than the previous estimated cost of the epidemic.
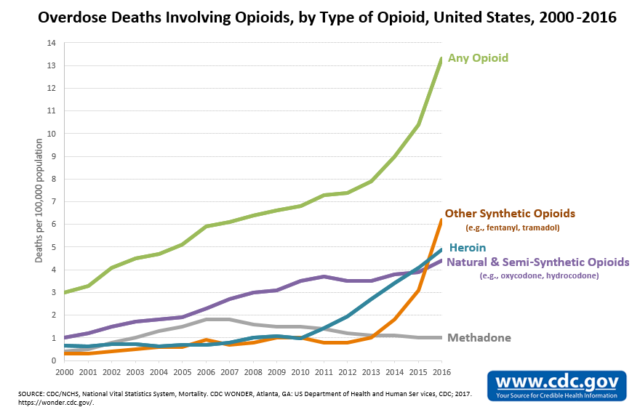
Prescription opioids are a particular problem. According to the Centers for Disease Control and Prevention (CDC), prescription opioids are a key contributor to the opioid epidemic in the United States, accounting for more than 40% of all U.S. opioid overdose deaths in 2016, with more than 46 people dying every day from overdoses involving prescription opioids.
In Philadelphia, the impact of the opoioid epidemic has been devastating. According to the city’s Department of Health, fatal drug overdoses from 2013-2015 increased by more than 50%, from 459 deaths to 702. During 2015, Philadelphia experienced more than twice as many deaths from drug overdose than from homicide. Eighty percent (80%) of these involved opioids.
What’s to be Done?
Recently, the Healthcare Leadership Network of the Delaware Valley convened a CEO Roundtable, hosted by Cooper University Health System, on what can be done to deal with the many challenges posed by the opioid epidemic. The panel discussion sought to offer perspectives from clinical, public health, governmental policy, health system and evidence-based treatment points of view. The general consensus – there were many contributing factors to the problem and it will take a dedicated commitment of coordinated effort to bring about an effective solution.
Dr. Susan Freeman, President & CEO of Temple University’s Center for Population Health, described her organization’s approach as an “all hands on deck” effort to address many of the multi-faceted issues exacerbated by opioid abuse. Temple’s Substance Abuse Task Force Action Plan, for example, focuses on six primary areas:
- Building trust with patients/substance abusers
- Ceasing addiction
- Proactively identifying patients at risk
- Reviewing physician prescription practices
- Education and research
- Partnerships with entities such as the Philadelphia Department of Health and other like-minded organizations.
Focus on Families
Similarly, Douglas Tieman, president & CEO of Caron Treatment Centers, noted it’s important to remember that substance abuse is a chronic disease that doesn’t end after a 28-day rehab visit. The most effective treatments are multi-disciplinary, including medication-assisted therapy, bio-psycho-social treatment, evidence-based treatment programs such as motivational interviewing, 12-step integration, trauma and family counseling, and a continuing care plan to lessen the chances of recidivism.
Such integrated approaches can have long-term positive effects. If behavioral health, substance abuse and mental health issues are treated in time, “the costs of other health-related issues go way down as well,” he said.
Even so, getting patients and families to participate in long-term programs can be a challenge in itself.
“We live in a microwave society that wants everything immediately,” noted Alan Oberman, CEO of John Brooks Recovery Center. “Most families, unfortunately are dealing with a ‘crisis of now’ and aren’t willing to listen to discussions of long-term chronic issues.”
A Center for Healing
Adrienne Kirby, PhD and chairman and CEO of Cooper University Health Care, said her long-term goal was to create at Cooper a “center for healing” that would address many of the related factors that contribute to problems faced by substance abusers. She said Cooper has been on the front lines, working with Camden County Police, to identify and reach out to patients in need. She said intervention needs to be combined with treatment, as well as other support services, such as housing.
Another key aspect of Cooper Health’s approach is to upgrade the curriculum so that students, residents, as well as faculty, are trained to recognize and treat substance abuse patients effectively.
Information is Key
A key challenge to implementing a coordinated strategy is the sharing of information. In addition to HIPAA regulations, the infrastructure simply doesn’t exist yet to allow the exchange of bio-social information among health care entities and community-based support organizations.
“We don’t have the infrastructure for mental health that we have in physical health,” said Dr. Kirby. “The law doesn’t allow us to be there yet.”
Nevertheless, such an information-sharing capability could help ensure that substance abuse patients receive the continuing care and social support they need. For example, with patients’ permission, telemedicine apps could combine with GPS to manage patients’ long-term illnesses, monitor their activities and ensure they are complying with what is needed to maintain a healthy recovery.
Information can be even more important in terms of prevention – stopping substance abusers before they get started. Caron, for example, works with 600 grade schools and high schools to educate students about the dangers of substance abuse. According to Caron’s Tieman, if students can be persuaded to postpone their introduction to alcohol, marijuana and other substances, it can significantly delay the onset of substance abuse.
There is no panacea. The opioid epidemic has been years in the making and will no doubt take years to overcome. In the meantime, healthcare communicators who work with organizations involved in the issue need to keep abreast of news and developments so they can provide their respective audiences with timely information and advice.